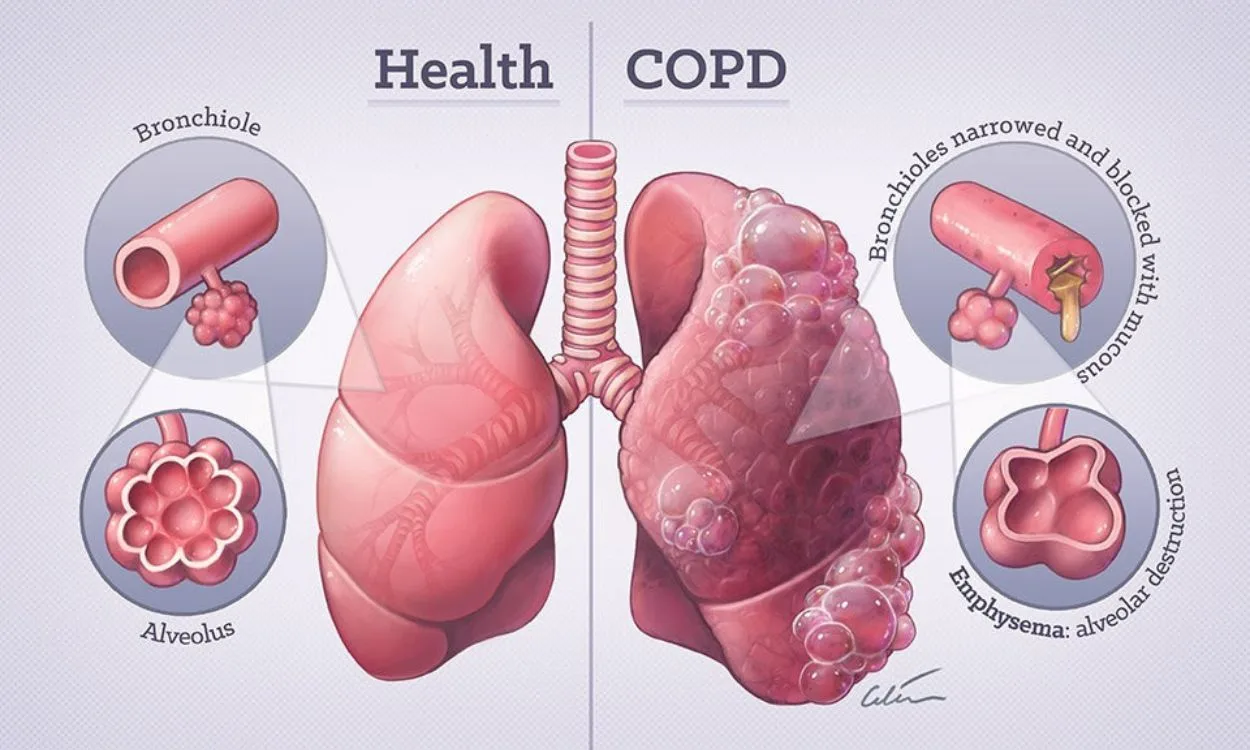
Diagnosing Chronic Obstructive Pulmonary Disease (COPD) involves a comprehensive approach that combines medical history, physical examination, and various tests to assess lung function and rule out other possible conditions. COPD is a progressive lung disease characterize by airflow limitation, typically associate with chronic bronchitis and emphysema.
One of the key tools use in managing COPD is bronchodilator therapy, often deliver through inhalers like Asthalin, which contain medications such as salbutamol to relieve symptoms and improve airflow. This essay will delve into the diagnostic process of COPD, focusing on the role of Asthalin inhalers in both diagnosis and management.
Medical history plays a crucial role in diagnosing COPD. Healthcare providers inquire about symptoms such as chronic cough, sputum production, shortness of breath, and exposure to risk factors such as smoking, occupational dust, or indoor air pollution. Patients’ smoking history, including duration and intensity, is particularly relevant as smoking is the primary risk factor for COPD. Additionally, any history of respiratory infections or exacerbations provides valuable insights into the progression and severity of the disease.
Physical examination helps healthcare providers assess the patient’s respiratory status. They may observe signs such as wheezing, diminish breath sounds, and purse-lip breathing, indicative of airway obstruction and hyperinflation. Cyanosis, clubbing of the fingers, and peripheral edema may also be present in advance stages of COPD. However, it’s important to note that physical examination findings alone are not sufficient for a definitive diagnosis of COPD.
Pulmonary function tests (PFTs) are essential for confirming the diagnosis of COPD and evaluating its severity. The most common PFT is spirometry, which measures the volume and flow of air during breathing maneuvers. Patients are ask to take a deep breath and then exhale forcefully into a spirometer.
Spirometry assesses parameters such as forced expiratory volume in one second (FEV1) and force vital capacity (FVC). In COPD, airflow limitation leads to decreased FEV1/FVC ratio, often less than 0.70, indicating obstruction. Reversibility testing with a bronchodilator, such as salbutamol found in asthalin inhaler can help differentiate COPD from asthma.
If there is a significant improvement in FEV1 after bronchodilator administration, it suggests a component of reversible airway obstruction, which is more consistent with asthma than COPD.
Furthermore, the diagnosis of COPD is not solely base on a single test or symptom but rather on the integration of multiple clinical and laboratory findings. Patient education also forms an essential component of COPD management, as it empowers individuals to recognize symptoms, adhere to treatment regimens, and make lifestyle modifications to minimize disease progression and exacerbations.
As part of the diagnostic process, healthcare providers must also consider alternative diagnoses that may mimic COPD. Conditions such as asthma, congestive heart failure, bronchiectasis, and pulmonary fibrosis can present with similar symptoms of dyspnea and cough.
Distinguishing between these conditions requires careful evaluation of clinical features, imaging studies, and pulmonary function tests, as well as response to specific therapies such as bronchodilators and corticosteroids.
The role of Asthalin inhalers extends beyond their use in diagnosing and managing COPD. These inhalers are also instrumental in preventing and treating exacerbations, which are acute worsening of symptoms often trigger by respiratory infections or environmental factors.
Prompt initiation of bronchodilator therapy, including the use of Asthalin inhalers, can help alleviate bronchoconstriction and improve lung function during exacerbations, thereby reducing the need for hospitalization and corticosteroid therapy.
In addition to bronchodilators, inheal corticosteroids (ICS) are frequently use in the management of COPD, particularly in patients with frequent exacerbations or severe airflow limitation. Combining ICS with long-acting bronchodilators in a single inhaler device offers the convenience of dual therapy and may improve symptom control and lung function.
However, the use of ICS in COPD is not without controversy, as prolong exposure to corticosteroids may increase the risk of pneumonia, osteoporosis, and other systemic side effects.
Other pharmacologic interventions for COPD include long-acting muscarinic antagonists (LAMA) and long-acting beta-agonists (LABA), which provide sustain bronchodilation and symptom relief.
Combination therapy with LAMA/LABA or triple therapy with LAMA/LABA/ICS is recommend for patients with persistent symptoms despite monotherapy or for those at high risk of exacerbations. The selection of pharmacologic agents is guide by disease severity, symptom burden, exacerbation history, and individual patient preferences.
In addition to pharmacologic therapy, non-pharmacologic interventions play a crucial role in COPD management. Smoking cessation remains the single most effective strategy to slow disease progression and reduce mortality in COPD. Healthcare providers should offer smoking cessation counseling and support to all patients with COPD, emphasizing the importance of quitting smoking to improve symptoms and prolong survival.
Pulmonary rehabilitation is another cornerstone of COPD management, involving a multidisciplinary approach that integrates exercise training, education, nutritional support, and psychosocial interventions. Pulmonary rehabilitation programs have been shown to improve exercise capacity, dyspnea, and quality of life in patients with COPD, leading to reduce healthcare utilization and mortality.
Furthermore, vaccination against influenza and pneumococcal infections is recommend for all patients with COPD to reduce the risk of respiratory infections and exacerbations. Annual influenza vaccination helps prevent seasonal flu-relate complications, while pneumococcal vaccination reduces the incidence of pneumococcal pneumonia and its associate morbidity and mortality.
In addition to spirometry, other tests may be perform to assess lung function and help guide treatment decisions. These include lung volume measurements, such as plethysmography and gas diffusion tests, which evaluate the extent of hyperinflation and gas exchange abnormalities in COPD. Arterial blood gas analysis provides information about oxygenation and carbon dioxide retention, which is important in severe cases of COPD or during exacerbations.
Imaging studies such as chest X-rays and compute tomography (CT) scans are valuable tools in diagnosing COPD and evaluating its complications. Chest X-rays may reveal hyperinflation, flatten diaphragms, and signs of comorbid conditions such as pneumonia or lung cancer. CT scans offer more detail images of the lungs and can detect emphysema, bronchial wall thickening, and bronchiectasis. These imaging modalities help assess the extent of lung damage and guide treatment decisions, particularly in candidates for surgical interventions like lung volume reduction surgery or lung transplantation.
Beyond objective testing, the response to bronchodilator therapy provides further diagnostic and prognostic information in COPD. Short-acting bronchodilators, such as salbutamol, are often used as rescue medications to relieve acute symptoms of bronchoconstriction and dyspnea. Patients with COPD may experience significant improvement in symptoms and lung function following bronchodilator administration. This response helps confirm the presence of reversible airway obstruction, which is more common in asthma but can also occur in COPD, particularly in its early stages or during exacerbations.
The use of Asthalin inhalers containing salbutamol is integral in both the diagnostic process and management of COPD. These inhalers provide rapid relief of bronchoconstriction by activating beta-2 adrenergic receptors in the airway smooth muscle, leading to bronchodilation and improve airflow. The response to bronchodilator therapy, assess through spirometry or symptom improvement, helps differentiate COPD from other respiratory conditions such as asthma and bronchiectasis.
In addition to its diagnostic role, Asthalin inhalers are a cornerstone of COPD management. They are commonly prescribe as rescue medications for acute symptom relief and as part of maintenance therapy in combination with long-acting bronchodilators and inheal corticosteroids. Asthalin inhalers offer convenience and ease of use, allowing patients to self-administer medication as need to alleviate symptoms of dyspnea and improve exercise tolerance.
However, it’s important to recognize that while bronchodilators like salbutamol provide symptomatic relief, they do not modify the underlying disease process in COPD. Therefore, a comprehensive treatment approach also includes smoking cessation, pulmonary rehabilitation, vaccinations, and pharmacologic interventions aim at reducing exacerbations and improving quality of life.
In conclusion, diagnosing COPD involves a multi facet approach that integrates medical history, physical examination, pulmonary function tests, imaging studies, and response to bronchodilator therapy.
Asthalin inhalers containing salbutamol play a pivotal role in both the diagnostic process and management of COPD, providing rapid relief of bronchoconstriction and improving symptoms of dyspnea.
By incorporating these tools and interventions, healthcare providers can accurately diagnose COPD, assess its severity, and develop individualize treatment plans to optimize patient outcomes and quality of life.